Category: Business
First in a Board-Level Series Guiding Hospitals Toward Safe, Equitable, and ROI-Driven AI Deployment
Black Book survey reveals just 1 in 4 hospitals can fully exchange patient data across national boundaries in Q4 2025
Far beyond Telehealth, this Black Book end-of-week flash survey of 152 healthcare executives reveals hospitals, physician groups, and diagnostics centers are accelerating claims, standing up RCM war rooms, stockpiling supplies, and freezing IT changes to preserve cash and continuity.
Independent national survey also recognizes Knowtion Health's HIM & Coding documentation support in denial recovery and appeals management.
Insights from Black Book's 12th Annual Healthcare Supply Chain and Purchasing Technology Leadership Surveys
30 Category Leaders named in Black Book Research's 12th Annual Healthcare Supply Chain Management User Surveys
Vendor Satisfaction Ratings Reveal RapidClaims Leads Across Key Operational and Financial Performance Metrics
New Gratis 35 Page Report to Health Systems Stakeholders Spotlights Risks to Reimbursement, Digital Mandates, Equity Initiatives, and Workforce Stability
Black Book Flash Poll Reveals Serious Concerns About Workforce Instability and Care Disruptions Across Hospitals, Nursing Homes, and Long-Term Care Facilities
Healthcare Executives Highlight Ongoing Critical Gaps in Patient Identity Management, Eligibility Verification, Charge Capture Accuracy and Denial Processing, Underscoring the Urgent Need for Comprehensive Interoperability Solutions
EnableComp, XTend Healthcare, Cedar, Knowtion Health, and others recognized as top performers in ten distinct AR categories, as health systems and providers acknowledge that complex AR recovery is not a one-size-fits-all challenge
Huron, ECG, and SimiTree score highest in client satisfaction as demand surges for consulting in denials prevention, outsourcing transitions, and enterprise-wide AI readiness
As Financial Margins Shrink and AI Transforms Operations, RCM Outsourcing Emerges as a Strategic Imperative for Providers Seeking Stability, Scalability and Performance

Newly Enhanced Key Performance Indicators Set Industry Standard for Evaluating Revenue Cycle Technology and Managed Service Vendors

Pandemic-Era Boom Fades as Digital Health Founders Warn of Funding Pressures, Operational Overreach, and Growing Demand for Measurable ROI

Independent Investor Poll Highlights Top-Ranked Startups Based on Strategic Growth Potential, Regulatory Readiness, and Clinical Impact Across the Continent

Health Plans and Payers Align Around VBRO Technology to Meet CMS Payment Reform Demands; Top-Rated Vendors Identified for Impactful Results
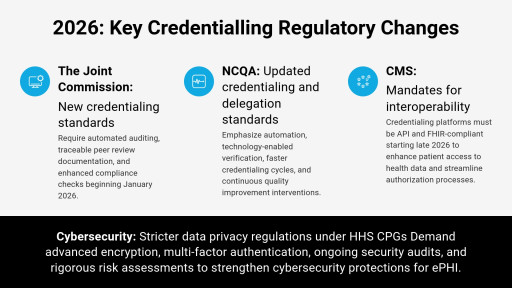
Survey Highlights Immediate Steps Needed for Health Systems to Ensure Readiness, Cybersecurity, and Operational Preparedness
Amid global expansion, Black Book advances its trusted, independent research model-implementing AI-powered KPIs, longitudinal client tracking, and purpose-built surveys tailored to virtual care, value-based delivery, workforce shifts, and emerging technologies for providers, payers, IT users, media, and investors
Poll Reveals Eight in Ten Healthcare Providers Are Reassessing RCM Managed Services Contracts Amid Growing Adoption of Intelligent Automation

New survey insights from Brazilian healthcare leaders highlight financial, regulatory, and interoperability barriers limiting EHR expansion despite significant investments.

From Cost-Cutting to Core Strategy: "Managed Services" Becomes Healthcare's New Operating System

Despite overwhelming public and industry support, federal action to prevent workplace violence in hospitals remains stalled in Congress, leaving frontline caregivers unprotected amid rising daily injury rates.
U.S. Healthcare Consumers Share Real-World Perspectives on Digital Tools, Communication Preferences, and Engagement Experiences in Black Book's Q1 2025 Sentiment Survey



Survey Reveals Global Healthcare Buyers Shifting IT Purchases to Regional Providers Amid Regulatory and Geopolitical Concerns

Over 900 healthcare technology experts identified key data systems that fail to deliver ROI and siphon funds from providers after implementation. In 2024, U.S. respondents reported that compounding inefficiencies, system downtimes, and ineffective health IT integration have driven total industry losses to over $8 billion annually, a sharp increase from $1.7 billion in 2017.

Management representatives from 1,428 provider organizations are electing to deflect mounting solution delivery concerns to outsourcing vendors, according to 91% of respondents to the sweeping annual poll of nearly 16,000 hospital and physician organizations across 40 categories of managed services.
The market research and data platform company also ranked in the top 15 of the list's healthcare industry services firms for three-year growth.

The technology and services insights firm again claims the honor as a member of the coveted Inc. Magazine list, citing continued sales growth exceeding three hundred percent.
Cerner is recognized as the top-rated inpatient EHR vendor for integrated hospitals and health delivery systems for the second consecutive year in ratings gathered exclusively from departmental clinical, financial, medical, and IT/operational staff members of hospitals, clinics and ancillaries providers. Cerner also was honored with the highest client experience scores in major Academic Medical Center health systems and affiliated providers in 2021, as in 2020.
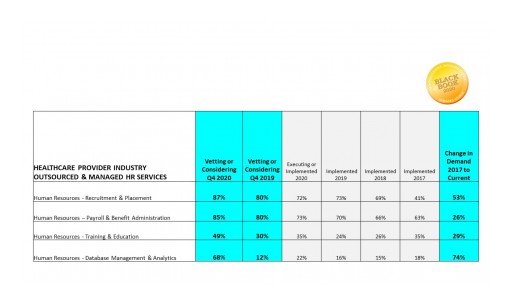
HR outsourcing in hospitals and physician groups has matured. Whether it's payroll, recruitment, data analytics or other overly stressed HR functions, a data-rich automated service underpinned by artificial intelligence is the key to successful HR transformation.

Hospital systems expenditure on protections as part of IT budgets increased 6% year-to-year but physician organization cybersecurity spend has decreased since 2018, and 92% lack full-time security staff.

Waystar, the merged solutions of ZirMed and Navicure, is the highest customer-rated comprehensive medical RCM Software Technology

Black Book is ranked among the country's most dynamic businesses rising to #511 with 750% three-year growth
Integrated EHR PM RCM ICD10 vendor tools get top marks in the mined US outpatient market

The healthcare industry's competitive research and survey innovation firm debuts at #601 with an astounding three-year sales growth of 750%
Survey finds 96 percent of existing Paragon users 'confidently optimistic' that Allscripts' acquisition will improve processes and benefit their organizations.
Sweeping survey of IT leaders reveals most small and mid cap companies remain significantly underinvested in data security innovation.
Outwardly great technologies are failing to have a penetrating effect on the healthcare system as patient IT adoption declined in 2017
Public Relations firms rated by client satisfaction and loyalty scores in eighteen key performance indicators by Payers and Providers
As the healthcare delivery industry deals with technology updates and implementations from ICD-10, EHR issues, physician alignment, big data, interoperability, value-based reimbursement reforms, decision support, revenue cycle, and patient marketplace shifts, hospital leaders embark on the major restructuring of hospital technology priorities and staffing alternatives for survival.
Black Book surveyed 738 emergency department administrative and nursing managers, and 1,104 ED physicians (over half are members of the American College of Emergency Physicians). 89% of ED leaders believe their hospitals rushed to purchase new EHRs and ED systems between 2010 and 2013 for meaningful use dollars, just to see productivity fall, liability rise and connectivity stall.
Different times or circumstances call for different leadership skills. As the healthcare industry implements radically innovative technologies, organizations are finding their incumbent senior management teams, regardless if CEOs, CFOs, etc. are lacking a skill set of successful EHR and population health deployments, analytics proficiency, and technology expertise outside of the CIO's office.
Hospital viability is now vulnerably reliant on the success of a single organizational venture: financial system transformation. As the healthcare delivery industry deals with ICD-10, EHR issues, physician alignment, population health, interoperability, value-based reimbursement reforms, and decision support, CFOs embark on the major restructuring of hospital technology priorities for survival.
